In response to the ongoing COVID-19 public health emergency, the Centers for Medicare & Medicaid Services (CMS) has broadened access to Medicare telehealth services to allow Medicare beneficiaries to receive services from their physicians without having to travel to a healthcare facility. Effective March 6, 2020, Medicare will pay for office, hospital, and other visits furnished via telehealth across the country (including in the patient’s home). Additionally, healthcare providers may reduce or waive cost-sharing for certain telehealth visits paid by federal healthcare programs.
Prior to this waiver, Medicare could only pay for telehealth for rural patients receiving the service from a clinic, hospital, or certain other types of medical facilities. During the public health emergency, patients from all parts of the country may receive telehealth services without leaving their homes. Effective immediately, the HHS Office for Civil Rights (OCR) has waived applicable HIPAA prohibitions to allow health care providers to serve patients in good faith through everyday communications technologies, such as FaceTime or Skype. However, transmissions should not occur over “public” sites such as FaceBook Live.
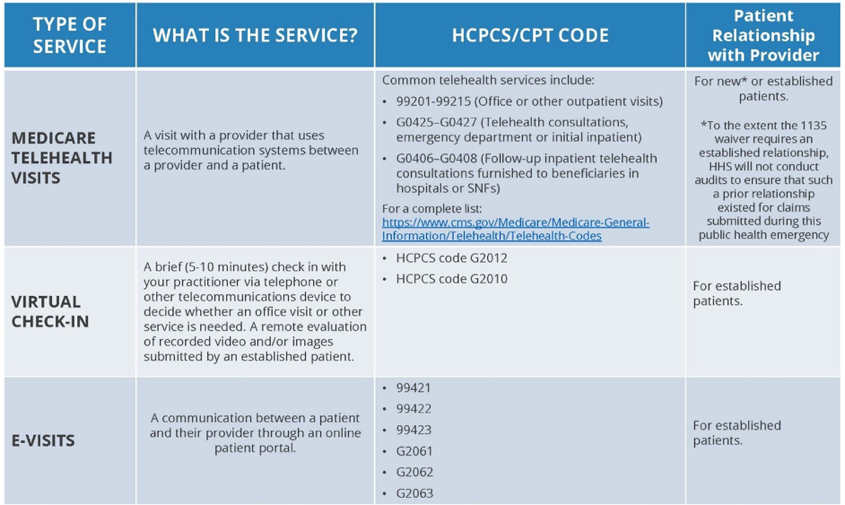
Note that these changes apply to Medicare only. CMS has urged Medicaid MCO’s to adopt similar policies and commercial payers are doing the same. Providers should regularly review TennCare MCO and commercial payer websites for each payer’s policies. There are actually three types of telehealth services, with varying rules for utilization and payment by Medicare:
-
- Medicare Telehealth Visits: Currently, Medicare patients may use telecommunications for office, hospital visits and other services that generally occur in-person. The key here is that the provider must use an interactive audio and video (FaceTime, Skype, etc.) that permits real-time communication between the provider office and the patient at home. To the extent that prior law required the patient have a prior established relationship with a particular provider, HHS will not conduct audits to ensure that such a prior relationship existed for claims submitted during this public health emergency. So new patients may use these telehealth services. These visits are considered the same as in-person visits and are paid at the same rate as regular, in-person visits.
- Virtual Check-Ins: Established Medicare patients in their home may have a brief “virtual” communication service with providers. These virtual services are expected to be initiated by the patient; however, CMS acknowledges that providers may need to educate beneficiaries on the availability of the service prior to patient initiation. Medicare pays for these “virtual check-ins” for patients to communicate with their doctors and avoid unnecessary trips to the doctor’s office. The provider may respond to the patient’s concern by telephone, audio/video, secure text messaging, email, or use of a patient portal. Standard co-insurance and deductibles apply. See HCPCS codes G2012 and G2010, as applicable.
- E-Visits Via Online Patient Portal: Established Medicare patients may have non-face-to-face patient-initiated communications with their doctors without going to the doctor’s office by using online patient portals. For these E-Visits, the patient must make the initial inquiry and communications can occur over a 7-day period. Use CPT codes 99421-99423 and HCPCS codes G2061-G2063, as applicable. The patient must verbally consent to receive virtual check-in services. The Medicare coinsurance and deductible would apply to these services.